

Idiopathic fibrosis of the conduction system After left anterior hemiblock, the next most common abnormality of the intraventricular conduction system is right bundle branch block, followed by left bundle branch block and left posterior fascicular block, or hemiblock. Left anterior fascicular block, or hemiblock, is the most commonly seen conduction abnormality of the intraventricular system with up to a 6% prevalence in the normal population. Congenital complete heart block has an incidence of one in 15,000 to 25,000 live births, with a 60% female predominance. The highest incidence of complete heart block is seen in the seventh decade, with a 60% male predominance. The P–R interval decreases and the Wenckebach block disappears with increased activity, and is considered normal vagal influence on the AV node.Īcquired complete heart block is rarely seen in young adults without heart disease. However, a longer P–R interval, and even Mobitz I (Wenckebach) block can be seen in young, well-conditioned individuals at rest and during sleep. History Part 2: Prevalence:įirst-degree AV block, with a P–R interval greater than 200 ms, is rarely found in young, healthy adults during activity. Concomitant structural heart disease, a wide QRS complex, or long Q–T interval increases the risk of symptoms in the congenital group.įlectrocardiogram (EKG) shows a constant P–nckebach) block, bundle branch blocks or fascicular blocks rarely produce symptoms. Children with congenital complete heart block are generally asymptomatic, but tend to develop symptoms as adults. Patients with acquired complete heart block or high-grade AV block with two or more nonconducted P waves in a row, are usually symptomatic. Ventricular tachycardia (due to long Q–T)įatigue, or decrease in exercise tolerance History Part I: Pattern Recognition: Hemodynamically important signs of AV block Diagnostic Confirmation: Are you sure your patient has AV Block? Clinical criteria for confirming significant AV clockĬomplete heart block or advanced AV block seen on an EKG or ambulatory monitoring in the presence of symptoms.īlock below the His-bundle or an HV internal >100 ms found during an invasive electrophysiology study in a patient with intermittent symptoms.Ĭauses of temporary or reversible AV block have been ruled out.Ī.
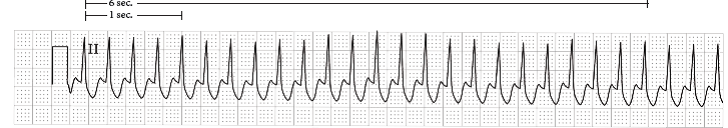
Left posterior fascicular block = left posterior hemiblock II. Left anterior fascicular block = left anterior hemiblock Third-degree AV block = complete heart block Type II second-degree AV block = Mobitz II block Type I second-degree AV block = Mobitz I block = Wenckebach block If AV block is symptomatic, and determined to be permanent, pacing is the only effective long-term therapy. Infra-Hisian block is the most important to identify, since it is the cause of most cases of symptomatic complete heart block.Īcquired AV block is most commonly caused by idiopathic fibrosis, acute myocardial infarction, or drug effects. Slowed conduction, or blocked conduction, can occur anywhere along the path of conduction fibers, and can generally be identified by EKG analysis.


 0 kommentar(er)
0 kommentar(er)
